Tips for Building Gut Health in Kids: Why Whole Foods are Best for the Microbiome
Contents
Breastfeeding vs. formula for your baby’s microbiome
As we age, the microbes that colonize our guts tend to stay for long periods of time. 1 Science is beginning to understand that these microbes have the potential to really shape our overall health, potentially even for the entirety of our adulthood. The foods we eat, and not the supplements we take, are the primary drivers of our microbiome health. This is true for kids and adults. Several postnatal studies have shown differences in microbiome composition between metropolitan areas of the United States versus rural villages in southern Malawai and Venezuela. 2 Differences have also been observed in babies who are raised on breast milk as compared to those who get formula. Breast-fed infants generally have a more uniform microbiome population when compared to formula-fed 3, and even supplementing with formula can shift the microbiome to a wider spectrum of microbes, which is common for formula-fed infants. 4 Now, for those of you who are thinking, “wait, if formula gives my baby a more diverse microbiome, that’s a good thing, right?” Not at the infant stage. For infants, you actually still want a less diverse microbiome because an infant’s immune system is just at the very start of development. Similar to how you slowly introduce babies to new foods, rather than throw it at them all at once so the body and newly formed immune system of newborns can develop at the correct pace.Probiotics in infant formula can help
The World Health Organization recommends breastfeeding exclusively for the first 6 months, but it’s not possible for all families. There have been several efforts to make formula that is similar to human milk by adding probiotics and prebiotics in hopes that it will help steer the development of proper immune function. 5 6 7 8 So far, the studies have shown that the microbiome of babies fed with pro and prebiotic formula look more like that of breastfed babies, though the jury is still out on whether there is real health improvement. 9 10 8 That said, two studies found that supplementation in preterm infants is linked with a reduced incidence of necrotizing enterocolitis and sepsis. 4 11 It’s the stage when babies are introduced to solid foods that we really see a high impact on the microbial population, with significant increases in Enterococci and Enterobacteria, and the appearance of Bacteroides, Clostridia, and other anaerobic Streptococci. 12 4 Somewhere between the first and third year of life, the microbiome starts to look a little more like that of an adult. This is where I want to talk a little more about why and how we should be looking toward probiotics and how important the effects of eating habits are on healthy growth and development for children.The microbiome and children’s growth
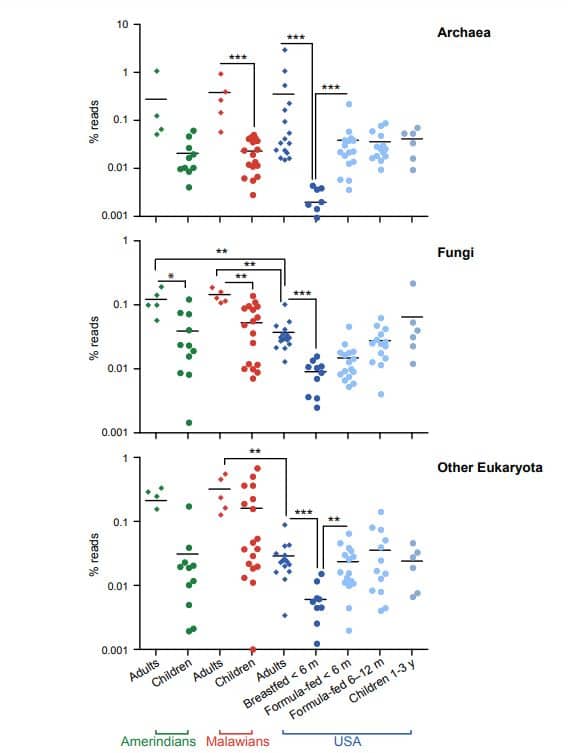
It’s been shown over the course of years of microbiome research that a well-rounded microbiome is key in human health — not just for adults, but for kids to achieve healthy growth. 13 14 15 A study done in 2014 comparing bottle-fed to breast-fed macaques showed that the breastfed infants had more memory T helper 17 cells (TH17), an important subset of immune cells that help protect us from pathogens and infection. 16 Alone, this data might not mean much to the average person, but the implication here is that the timing and foods that children are exposed to in their early life can have lasting consequences. The impact of the microbiota in children goes beyond just obesity or malnutrition, but into diseases such as asthma, dermatitis, chronic inflammatory disease, type 1 diabetes, and eczema, all which can last into adulthood. 17 18 19 Knowing how much our health is affected by our microbiomes, this makes me wonder what the American diet (access to highly processed foods and “quick” meals) means for our gut. A study carried out in 2011 by Jeffrey I. Gordon’s lab, looked at bacteria from 326 individuals from the ages of 0-17 and 202 adults 18-70 years of age and found that the composition of the microbiome starts to mature within three years following birth, something that Gordon found to be consistent throughout all three countries. In this same study, Gordon found that the Western lifestyle affects the bacteria makeup of our gut microbiome, from childhood into adulthood.The microbiome of Americans lacks diversity
On both graphs I’ve included, the blue dots or lines represent the number of different microbes in the American gut. The line graph discusses bacteria in particular, and really highlights how our gut bacteria as adults is less diverse compared to other countries. The dot graph aims to look at other microbes from different groups (Archaea, Fungi, etc.) and shows that the good Fungi and some other eukaryotes that also make up a healthy gut microbiome are much lower as well in America. The culprit of this is likely our diets, as these other countries don’t have as much access to the highly processed foods we eat here in the U.S. The sterile environment that we make these pre-packaged food in, plus that fact that they’re stripped of most nutrients, means that there’s hardly any good nutrition left, and as a result, they can start to feed some bad guys in the gut. Now, let’s dig in a bit further.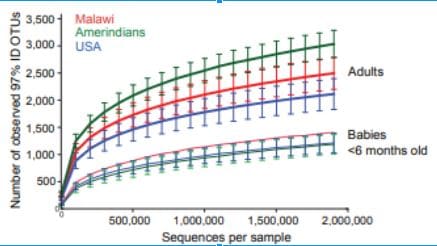
Probiotics (and prebiotics) are safe for children
For one, it’s pretty clear from several of the studies I linked to above that probiotics and prebiotics are safe for children. Breastfed babies are getting their good bacteria from Mom, but for those of us who can’t breastfeed, several groups are already working to include probiotics in formula. The particular strain that was studied was Lactobacillus rhamnosus GG (ATCC 53103). Another strain that has been tested is B. Infantis, which was demonstrated to reduce in instances of necrotizing enterocolitis (NEC) 20 and another study has tested a combination of probiotics in standard whey-based formula containing a total of 107 colony-forming units (CFU)/g of Bifidobacterium bifidum, Bifidobacterium breve, Bifidobacterium longum, B. longum subspecies infantis. This study supplemented infants with this combination of probiotics from 0 months to 12 months and found that supplementation changed the occurrence of specific bacterias and metabolites. However, a year after stopping probiotic intake, researchers looked at the fecal bacteria of the infants at age 24 months and did not see long-term effects on the microbiome after, or antibiotic uptake, which indicates that complementary probiotics are not just a one-and-done treatment and that the gut microbes need to be properly fed and kept up with in order to see the benefits. 21 Talk to your pediatrician about what the options are if this is a concern for you.Food Sources of Probiotics for Kids
When introducing solid foods to your child around age 4 to 6 months, instead of the jars of baby food you can buy at the grocery store, consider making them yourself at home. Following your pediatrician’s guidance, choose fresh organic fruits and veggies and invest in a good food processor. While fresh fruits and veggies aren’t a huge source of probiotics, they’re a wonderful source of prebiotic microbes and nutrients that your gut bacteria thrive on, which helps keep your colonies happy. Microbes thrive off of the sugars in complex plant polysaccharides (essential plant carbohydrates). For your bigger kids, look for yogurts that clearly state that they have probiotics included. Encourage fruits and veggies, and even consider letting them spend more time with pets, which can help the immune system mature. Fermented foods like what’s listed below are excellent sources of probiotics, but the flavors might be too strong for your little ones. Still, give these a try:- Unpasteurized sauerkraut
- Kimchi
- Miso
- Kefir
- Yogurt
- Soft cheeses
- Dairy products