Exploring Natural Prostatitis Remedies
Genes Mentioned
Contents
- Can treating gum disease cure prostatitis?
- Is prostatitis a sexually transmitted disease?
- Antibiotics and prostate problems
- Fungal study
- The prostate is prone to infection and inflammation
- Known prostatitis cures
- Quercetin study
- Berberine study
- H1 anti-histamines study
- Plant based study
- Exercise study
- Honorable mention
- Additional studies
- Top supplements for prostatitis
- Closing thoughts
This post is part of multi-part series shedding light on the latest treatments for common chronic conditions faced by an increasing number of Americans.
Prostate.
Just mentioning the word will get some snickers, but this little forgotten gland is crucial to every man’s health. In fact, if you are a man who would like to avoid getting cancer, the prostate is an excellent place to begin.
Approximately one in seven men will be diagnosed with prostate cancer at some point in their lifetime, and prostate cancer currently ranks as the third leading cause of cancer death for men behind only lung and colorectal cancer. Although this is a post about prostate inflammation and not prostate cancer, the principal is the same: men need to take care of their prostates from a relatively early age.
And while the vast majority of the research dollars go to prostate cancer, prostatitis, or chronic inflammation of the prostate, is often lost in the shuffle.
Yet, virtually all men will develop prostatitis at some point in their adult lifetime, and with symptoms ranging from frequent urination, to pelvic pain, and even erectile dysfunction, this disease should be on every man’s radar. 1 When you take a deep dive into the literature, it becomes clear that the umbrella term “prostatitis” actually represents multiple different infections and sources of inflammation.
As such, this post will offer a series of easy experiments men can perform at home to either better protect, or heal the prostate.
Can treating gum disease cure prostatitis?
However, before I dive into the meat of the research, I think it’s a good idea to start with an issue that everyone reading this can control for, and that’s dental hygiene.
As you’ll see reading this post, we get into issues of PH and which bacteria thrive in more acidic environments. For example, the PH of urine can dictate whether bacteria like E. coli can grow in the urinary tract. Similarly, the state of our dental hygiene also plays a role in the pathogenic load placed on the body. The issue first came on my radar when visiting with a holistic dentist recently. He developed a product that raises the PH of the mouth to make it more alkaline.
At first, I was skeptical (seems everyone is selling a supplement today), but then I did some reading.
I was surprised to see saliva referred to as containing many “host defense factors, and the PH of saliva is a biomarker for gum disease. 2 More acidic saliva correlates with more advanced gum disease, whereas more alkaline saliva is associated with better gum health.
But, here’s the kicker – gum disease and prostatitis go hand in hand. In fact, there are studies demonstrating significant improvement in prostate inflammation just by treating the gums alone. So, if you’re reading this and you have prostatitis, the first step is to visit with a holistic dentist, make sure your gums are healthy, and pay attention the acidity of your saliva.
Is prostatitis a sexually transmitted disease?
Yes, prostatitis can be contracted through sex, so the more sexual partners a man has, the higher his odds of developing the condition. 3 4 5 6 7
Interestingly, Trichomonas vaginalis, a parasite and STD, has been found in prostate biopsies of men with prostatitis, and although it seems that E. Coli is a much more regular culprit, the prostate’s susceptibility to Trichomonas vaginalis colonization has been linked to zinc levels. The prostate is the number one home for zinc in a man’s body, and when levels get low, studies have shown these types of pathogens can take a greater foothold.
Mineral deficiencies are common in the U.S., which means supplementing with small amounts of zinc (you don’t want to overdo it with zinc as large doses can cause side effects) to see whether conditions improve could be worthwhile. As far as food is concerned, pumpkin seeds and oysters are both high in zinc.
As an added benefit, zinc supplementation has also shown some promise in maintaining the cell lining of the gut, which can prevent or help to heal leaky gut, a condition that often accompanies prostatitis, and that is marked by a breakdown of the “epithelial” wall of the gut lining, which allows pathogens and undigested food particles to enter the blood stream. 8 9 I will touch more on leaky gut later in this post.
While we are putting a focus on Trichomonas vaginalis in this discussion about zinc, ultimately, identifying the exact pathogenic bacteria causing issues in the prostate can be difficult since samples are often contaminated by the bacteria that grow in the urethra.
Antibiotics and prostate problems
Prostatitis can be contracted from sexual activity, but the very antibiotics used to treat prostatitis can, in some cases, be the culprit behind chronic inflammation of the prostate.
Ruling out fungal infection
Consider this study which appeared in the Central European Journal of Urology. The authors found that most young men presenting with prostatitis, who also had low prostate specific antigen (PSA) numbers (higher PSA means greater likelihood of prostate cancer), were suffering from a yeast infection, not bacterial prostatitis, although E. Coli was thought to be the “bridge” that brought yeast to the prostate region in the first place.
Fungal study
| Type | Fungal |
|---|---|
| Size | 1,000 men |
| Treatment | Fluconazole, potassium citrate |
| Diet changes | Low carb |
| Results | 80% saw improvement in symptoms |
This tiny study had the same finding, but in this case, biopsies showed dual contamination with Candida Albicans and Trichomonas vaginalis.
So, as a preliminary matter, if you’re a young man suffering from what you think could be prostatitis, have your PSA labs done. Bacterial prostatitis can raise PSA numbers, so if you have low PSA numbers, you may be looking at an anti-fungal regimen rather than a course of antibiotics.
Broad-spectrum antibiotics, which is the solution offered by most urologists, will only serve to further destroy the microbial balance in the gut and urinary tract, making it that much easier for the yeast to spread. In these cases, loading up on antibiotics will only make matters worse.
An easy experiment to run if you suspect a fungal issue is to go on a type of Candida protocol for about 10 days and see how your body responds. In essence, this will involve eating zero sugar and following a low glycemic diet (meaning very low carb but NOT zero carbs).
Don’t go “keto” or zero carb as studies show that yeast can survive very effectively on ketones.
If these dietary changes provide relief, you have a decent idea that the problem is fungal in origin, especially if you have low PSA numbers. It is also a good idea to have a mycotoxin panel done to identify potential issues with toxic mold.
The Central European Journal of Urology study used fluconazole, but some men may better tolerate nystatin.
I would also note that the mechanistic justification for the low carbohydrate and anti-fungal diet in the Central European Journal of Urology could actually justify two experiments. The one I list above is the anti-fungal-diet option (very low carb), which is proven in a well designed study, however, what seems to have been lost in that approach is the suggestion that E. coli was the bridge that allowed for the invasion of Candida in the first place. The low carbohydrate diet cuts off the fuel source for Candida growth, but doesn’t address the possible source of the E. coli.
Based on the studies I cite below in the plant based protocol section of this post, it could just as easily be argued that a diet, like many plant based protocols, that work to make the urine more alkaline could be just as effective, if not more so, at healing cases of prostatitis, since the rise in urine PH would remove the fuel source for E. coli (which thrives in acidic urine) and therefore remove the “fungal bridge” to the urogenital region. In the European study, the researchers gave the subjects potassium citrate to make urine more alkaline.
The prostate is prone to infection and inflammation
The prostate sits in an anatomical position, wrapped around the urethra, and close to the rectum, that is ripe for infection.
Infection causes inflammation. 10 When the prostate is inflamed, it can become enlarged, putting pressure on the urethra and, in some cases, making it more difficult to fully empty the bladder. Urine then gets trapped and backs up, which can contribute to lingering low grade infection, even where tests come back negative.
The role of leaky gut
In addition to the retention of urine, the prostate can become infected due to a break down in the intestinal lining, sometimes called “leaky gut.”
Leaky gut is characterized by bacteria, toxins, and even undigested food, which are all meant to stay within the digestive system, leaking out into the blood stream where these invaders have the potential to cause autoimmune like reactions in some people.11
For example, men who give up gluten sometimes find that their prostate issues go away.
Presumably, this happens because gluten increases the production of zonulin, a protein that is responsible for breaking down the “intracellular tight junctions” that form the gut wall. 12 Removing gluten reduces levels of zonulin, which allows the gut to heal, stopping the release of irritants that had previously reached the blood stream where they can cause autoimmune reactions.
As a practical matter, this will overlap with the anti-fungal protocol above, but stop eating gluten for a month and see if the condition improves. There are multiple anecdotal stories online about men healing prostate issues by cutting out gluten.
And while the Paleo community has done an excellent job tagging grains as the cause of leaky gut, the reality is more complex for most men. Yes, grains, especially refined grains, can feed yeast and are contraindicated on an anti-fungal protocol, but some men will also do well to avoid saturated fat, as saturated fat has been linked to intestinal permeability as well. 13 While the saturated fat study I cite here was a study performed in mice, it’s worth mentioning because many with mast cell issues don’t respond well to high fat diets and foods, and one of the theories I will advance later in this post discusses the possibility that prostatitis is an autoimmune condition for a good number of men.
The point here is that a low-grade infection of the prostate can come from places you may not expect, including the gut.
Hidden infection
Most people have cancerous cells in their bodies, but they do not have “cancer.” The principal is the same with infection. A urologist may tell a man with prostate issues that he has no infection, but as I alluded to above, that doesn’t mean there aren’t bad bacteria present in the region that are causing problems.
However, it is important to point out that many men have identifiable infection that can be detected through lab tests.
This quote from the Journal of Clinical Microbiology Reviews is instructive:
While it is difficult to definitively extrapolate from animal models, antibiotic pharmokinetic studies with a murine model have suggested that treatment failures in chronic prostatitis are probably a result of the local microenvironment surrounding the persistent focal and well-protected small bacterial biofilms buried within the prostate gland. These conclusions support the molecular and culture data implicating bacteria as a cause of chronic idiopathic prostatitis.
As a result, the first course of treatment for men who complain of prostatitis is antibiotics.
However, antibiotics cannot penetrate the prostate effectively. Forums are full of men who claim to have had some temporary relief from antibiotic use, only to have symptoms return when antibiotics stop. This can likely be explained by the fact hat the antibiotics temporarily lower the pathogenic load in the region, but don’t address the underlying cause of the disease in the first place. Ironically, and as the studies on yeast infections above demonstrate, antibiotic use may be one of the primary contributing factors to long battles with prostatitis.
To be fair, antibiotics may have efficacy for men suffering with an acute infection. However, for chronic repeat sufferers, antibiotics are not a cure, because, as the Journal of Clinical Microbiology states, bacteria can thrive in a prostate not receiving proper blood flow due to bacteria fortified in biofilm. 14
It’s now time to bring nitric oxide into the equation.
Nitric oxide and blood flow
The blood vessels in the prostate are the smallest and most delicate in the body.
Nitric oxide (“NO”) causes blood vessels to relax so they can receive oxygenated blood. The popular erectile dysfunction drugs Cialis and Viagra work because they flood NO into the prostate region (also relieving symptoms of BPH). 15
NO is anti-pathogenic, but unfortunately, infection reduces BH4, a chemical the body needs to make NO. 16 In addition, fungal pathogens cause an uptick in the production of uric acid in the body, and high levels of uric acid also prevent the synthesis of NO. 17
So, in essence, an infected prostate loses the ability to receive NO because the body uses BH4 to fight off the invaders, rather than to synthesize NO. The uric acid mediated disruption of NOS can come from the activity of the fungal pathogen OR it can be the result of a diet too high in animal protein and sugar, as well as the result of certain genetic “mutations.” It’s likely all three factors combine to form the serum uric acid levels of any given individual.
Therefore, lingering infection means lower NO bioavailability, reduced blood flow, and greater risk for infection, or greater risk for lingering infection to better protect itself with production of biofilm. 18 Reduced BH4 also results in a process known as NOS uncoupling, which produces the free radical superoxide instead of NO.
For more on the genetics of NO production, see our NOS3 gene page.
Whether you want to call it acute bacterial, or chronic nonbacterial, prostatitis is a recurrent inflammation of the prostate caused in part by chronic decline in nitric oxide bioavailability.
The recent literature suggests that the condition referred to as chronic idiopathic (nonbacterial) prostatitis may actually have an infectious etiology.
During the past few years, molecular data and cultures performed with special media (discussed below) strongly suggested that chronic idiopathic prostatitis may actually be a cryptic bacterial infection of the prostate gland that is usually missed or undetected by routine conventional cultures in clinical microbiology laboratories.
Journal of Clinical Microbiology
Decline in the anti-pathogenic NO results in poor blood flow to the prostate, which adds an anaerobic environment to a region that sits next to multiple potential sources of infection. The stage is then set for infection to settle in, with E. Coli being one of the biggest culprits.
It is for this reason that studies have shown that use of the ED drug Cialis, actually helps heal and reduce inflammation markers in the prostate. Flooding the region with NO, reduces cytokine activity. 19
Increase in mast cells irritate the prostate
Chronic infection causes inflammation.
In response to inflammation, the body produces a greater number of localized mast cells, which makes matters worse. 20 Mast cells are produced during times of stress, as well as in response to ingesting foods or substances that trigger an allergic response. 21
Therefore, mast cell production in the bladder and prostate is basically an allergic response to inflammation that can increase the inflammatory cycle and locally suppress the immune system. 22 Remember that when provoked by a stimulus perceived as a threat to the immune system, mast cells release histamine, as well as a whole host of other inflammatory compounds. After a long period of inflammation, which has caused mast cells to pool in the prostate area, seasonal allergies can contribute to symptoms. The mast cells are there in larger numbers and will release their inflammatory cocktail in greater concentrations in areas of the body that are perceived as under attack.
I’ve written previously about pollen allergies causing anxiety, but presumably they can contribute to some types of prostatitis as well.
I get into a study focusing on an autoimmune model of prostatitis in a couple paragraphs, but many people with mast cell issues don’t do well with red meat, pork, and high fat diets. If you have allergies, cutting out saturated fat and going on more of a plant based diet for awhile could be helpful.
Known prostatitis cures
Applying the prostate facts
Ok, so we’ve offered three overarching reasons for prostate problems:
- Anatomical position close to sources of infection (vulnerable to leaky gut)
- Small blood vessels sensitive to declines in NO
- Mast cell / autoimmune reaction to allergens, infection, stress
Let’s now take these three theories and apply them to the best prostatitis studies.
Quercetin
Quercetin is a mast cell stabilizer and biofilm disrupter.
Knowing this, it’s not a surprise that studies show quercetin significantly reduces symptoms of prostatitis, especially when it’s paired with bromelain, an enzyme found in pineapple juice that increases the bioavailability of quercetin. Both quercetin and bromelain act as natural antihistamines, which reduces mast cell count and eases symptoms.23 Quercetin has also been shown to increase NO levels and improve endothelial function. 24
This double blind, placebo controlled study found that quercetin and bromelain to be effective at treating prostatitis.
Quercetin study
| Type | Chronic non-bacterial |
|---|---|
| Size | 28 men |
| Treatment | Quercetin 500mg twice daily, and then twice daily combined with bromelain |
| Diet changes | None |
| Results | 67% of quercetin takers had improvement of at least 25% |
Quercetin fits under the three prostate rules listed above both as a mast cell stabilizer and a biofilm disrupter.
A note on prostatitis and genetics (technical)
At a genetic level there isn’t much data out there for potential markers related to prostatitis, although SOD2 SNPs and other endogenous may play a role. One interesting study from 2002 did highlight some potential markers and interestingly identified differential treatment responses based on genetics.
The risk allele ‘A’ of rs1800896 in the IL10 gene is associated with a reduction in levels of IL-10 protein. IL-10 is a major anti-inflammatory cytokine, a protein released by cells which helps damp down the inflammatory response, and so a lack of its expression is therefore associated with chronic inflammatory disorders.
The 2002 study in patients with chronic prostatitis found that men with prostatitis were more likely to have a low IL-10 producing genotype, “suggesting autoimmunity as a potential etiology.” So, check another box for our mast cell rule there.
Interestingly, the authors also noticed that those with the “normal” ‘G’ allele of rs1800896, who also carried the risk ‘A’ allele of rs1800629 in the TNFA gene responded poorly to quercetin treatment. Which may somewhat explain the differences seen in quercetin treatment studies.
Berberine
Berberine, which I have written about previously as an anti-cancer supplement, has been shown in some animal studies to cure prostatitis. 25
Berberine study
| Type | Chronic non-bacterial |
|---|---|
| Size | N/A, study performed in rats |
| Treatment | Berberine (Note: Epithelial (gut) degeneration observed in rats with CNBP. Histidine metabolism observed as an issue contributing to CNBP. Berberine may be protective against CNBP because it resets disruptions in metabolic pathways associated with the condition.) |
| Diet changes | N/A |
| Results | Berberine reduced gut inflammation and reset metabolic pathways, which helped with CNBP |
There is a community of functional medicine doctors, the most vocal being Dr. Dach in South Florida, who believe that berberine heals leaky gut. Healing of leaky gut, presumably by wiping out pathogenic bacteria, closes the doorway for bad bacteria to enter the blood stream and infect the prostate.
Berberine is anti-fungal and antimicrobial. It fits nicely within our three rules for prostate health listed above.
As an added benefit, berberine has been proven as a prostate healthy supplement in the context of prostate cancer where it inhibited growth of prostate cancer cells. 26
Antihistamines – prostate allergy?
To further advance this theory, this study in the Journal of Urology found that taking H1 antagonists, like Zyrtec or Claritin, helped alleviate prostatitis. Why? Just as the quercetin did, the antihistamine reduced mast cell count, thus dialing back inflammation. Genetics wise, those with AOC1 “mutations” can be more prone to histamine issues.
H1 anti-histamines study
| Type | Autoimmune, mast cell |
|---|---|
| Size | Unknown |
| Treatment | H1 anti-histamines, testing for mast cell and nerve growth factor secretions in prostatic secretions |
| Diet changes | None |
| Results | Men with prostatitis showed increased mast cell tryptase and nerve growth factor in expressed prostatic secretions. Treatment of experimental autoimmune prostatitis with a mast cell stabilizer combined with a histamine 1 receptor antagonist resulted in a synergistic decrease in chronic pelvic pain |
Consider these two quotes:
Men with chronic pelvic pain syndrome showed increased mast cell tryptase and nerve growth factor in expressed prostatic secretions.
Treatment of experimental autoimmune prostatitis with a mast cell stabilizer combined with a histamine 1 receptor antagonist resulted in a synergistic decrease in chronic pelvic pain.
Antihistamines are mast cell stabilizers, again fitting nicely within our three rules.
Plant based diet
Try a plant based diet.
This study out of the University of Washington in St. Louis found that people with more acidic urine had greater likelihood of developing repeated urinary tract infections, especially those driven by E. Coli. Now think back to the yeast study I quoted above. The authors there believe that E. Coli was the bridge that allowed Candida and other pathogenic yeast to infect the prostate. As we don’t currently know exactly what causes prostatitis, it’s not a reach to assume that urinary tract infections could be present in symptomatic men. The UTI could then spread to the prostate or bladder, causing chronic problems. In fact, the urinary tract has its own microbiome, and certain strains of probiotics may play a role in staving off infection.
Plant based study
| Type | Urinary Tract Infection (UTI) |
|---|---|
| Size | Unknown |
| Treatment | Alkalize urine |
| Diet changes | None |
| Results | Those with more acidic urine at greater risk for recurrent UTI. Microbiome health also a factor. Acidic urine feeds E. Coli |
High animal protein diets cause greater acidity in the urine which allows for the invasion of bad bacteria, like E. Coli, that are linked to prostate inflammation.
If too much animal protein causes acidity that proliferates E. Coli, and eventually Candida, a plant based diet that makes the urine more alkaline could be a solution to prostate issues for some men. In fact, in addition to anti-fungal drugs, the yeast infection study gave subjects potassium citrate as a means for making the urine more alkaline, and the success rate there was over 80%. For more on how potassium citrate makes the urine more alkaline, see this University of Chicago article.
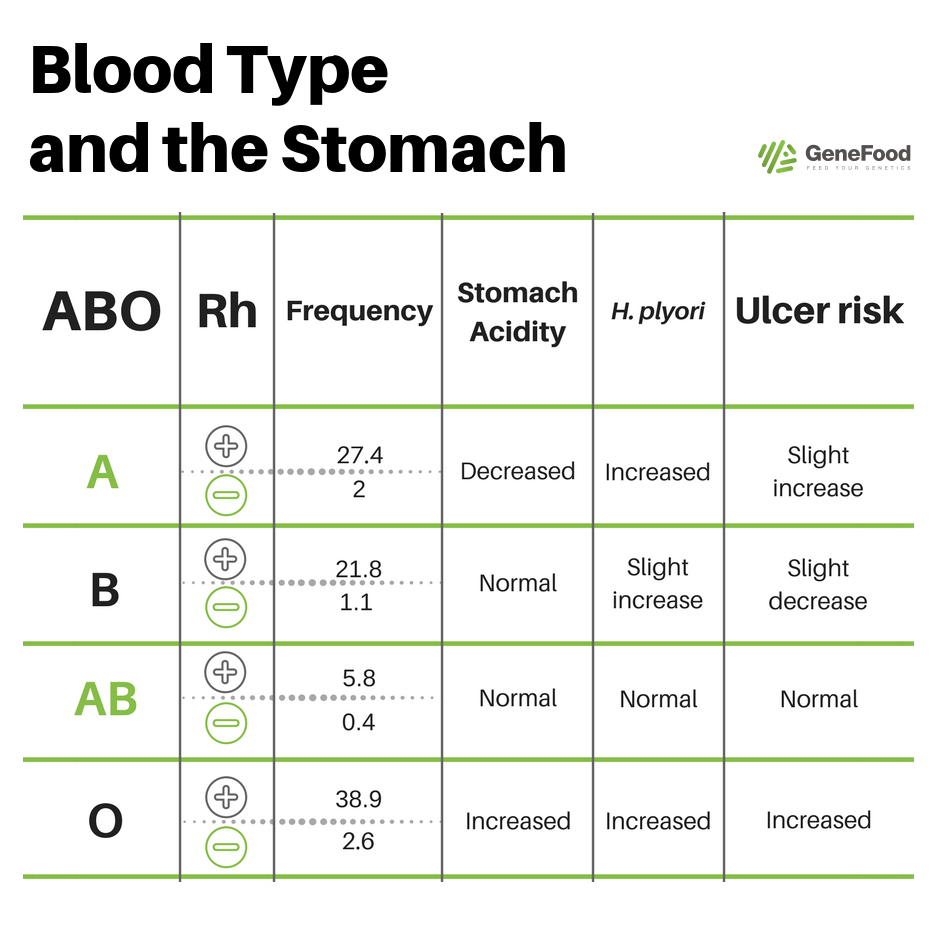
In this context, it is crucial to know your blood type. Although the blood type diet has largely been debunked, it contains one sound scientific principle, which is that blood type correlates to hydrochloric acid levels in the stomach. Type A, and A+ blood types have the lowest levels of hydrochloric acid with which to digest protein. A high protein diet in these individuals may leave undigested meat fermenting in the gut, which leads to pathogens, like E. Coli, that can cause problems for the urinary tract and prostate.27 28
Last, red meat in particular has been shown to be a problem for those with mast cell issues. If chronic inflammation, or some type of under the radar autoimmune condition, has caused a localized increase in mast cells or E. Coli infection, red meat and pork are definitely to be avoided.
Bottom line is that degraded gut health caused by too much animal protein will undoubtedly be a cause of poor prostate health for many men.
See also: Do plant based diets help us live longer?
Exercise
Exercise has been shown to increase NO and as I have written about previously, increase levels of butyrate, a short chain fatty acid that helps protect the lining of the gut.
In an Italian study, 231 sedentary men were put on an exercise regimen. Those who performed aerobic exercise saw greater relief than those who lifted weights.
Why?
Exercise study
| Type | Chronic non-bacterial |
|---|---|
| Size | 231 sedentary men |
| Treatment | Aerobic exercise and weights for 18 weeks total |
| Diet changes | None |
| Results | Both groups saw improvement, with the cardio group showing greatest results |
Well, this study also fits nicely within our paradigm. The increases in NO help with blood flow, and the cardio helps to repair the lining of the gut, degradation of which is a key factor contributing to the development of prostate infection.
Honorable mention
Additional studies that show promise treating prostatitis:
Additional studies
| Treatment | Mechanism | Type | Results |
|---|---|---|---|
| NAC (R) | Nrf2 / Biofilm | Rat study | Pain and inflammation reduced |
| Fluoroquinolones antibiotics, saw palmetto, lactobacillus sporogens, and Arbutin (R) | Reduction in Uropathogens | Human | Group using antibiotics plus natural supplements showed greatest reduction in symptoms |
| Nettles, saw palmetto, curcumin and quercetin blend plus antibiotic prulifloxacin (R) | Destroyed biofilms | Human | One month after treatment, 89.6% of patients who had received prulifloxacin and natural blend did not report any symptoms related to CBP, whilst only 27% of patients who received antibiotic therapy alone were recurrence-free |
Frequent sex
Ejaculation “drains” the prostate of stored fluid. When the prostate is becoming inflamed, or has a low grade infection, ejaculation gets rid of the bad stuff that is lingering and gives a “clean slate.” This is why you see some men with prostate issues get a “massage” which is a more thorough draining of the gland performed by a urologist, but those procedures come with risk of injury, so better to just have sex.
In fact, studies have shown that men who ejaculate more have lower incidence of prostate cancer.
Having said that, the issue of draining the prostate cuts two ways. In one sense, getting rid of stored fluid has shown promise for many men. However, let’s think back for a second to the discussion of zinc and Trichomonas vaginalis infection of the prostate, which seems to hinge on the zinc levels in that organ. You know what drains the prostate of zinc? You guessed it, ejaculating. So, it would seem, that at least for some men, excessive ejaculation, especially from masturbation since it offers very little in the way of, well, “benefits,” could be doing more harm than good. We do have studies that show that the prostate drained of zinc is more prone to infection.
Experiment: long term not ejaculating isn’t good for the prostate, but a short course, perhaps two weeks, of abstaining from what could be your favorite past time (while still engaging in sex) might do you some good, and give your prostate time to heal, if in fact it’s excessive masturbation that has been an irritant.
Note: some urologists would disagree that abstention from ejaculation improves zinc levels in the prostate. There are however, communities of men who swear by the practice, so I’ve offered the idea here as an experiment to consider if you’re facing a chronic case of inflammation you can’t seem to shake. See also this Reddit thread.
Top supplements for prostatitis
| Supplement | Study | Duration | Result | Notes |
|---|---|---|---|---|
| Quercetin | Quercetin in men with category III chronic prostatitis (R) | 1 month | 67% of quercetin takers had improvement of at least 25% | Quercetin and bromelain found to be effective at treating prostatitis |
| Berberine | Berberine Ameliorates Nonbacterial Prostatitis via Multi-Target Metabolic Network Regulation (R) | One week | Reduced gut inflammation and reset metabolic pathways in rats | Berberine may be protective against CNBP |
| Antihistamines | Role of mast cells in male chronic pelvic pain (R) | Unknown | Taking H1 antagonists, like Zyrtec or Claritin, helped alleviate prostatitis | Mast cells "may be potential targets for therapeutic intervention in men with chronic prostatitis/chronic pelvic pain syndrome" |
| NAC | N-acetylcysteine Ameliorates Prostatitis via miR-141 Regulating Keap1/Nrf2 Signaling (R) | Unknown | NAC relieved the carrageenan-induced CNP in rats | miR-141 inhibitor could reduce the effect of NAC on prostatitis |
| Saw palmetto, lactobacillus sporogens, and Arbutin with fluoroquinolones antibiotics | Chronic bacterial prostatitis: efficacy of short-lasting antibiotic therapy with prulifloxacin in association with saw palmetto extract, lactobacillus sporogens and arbutin (R) | 2 months | Antibiotic group combined with natural supplements saw most reduction in symptoms | Serenoa repens, lactobacillus sporogens and arbutin show better control and recurrence rate than antibiotics alone |
| Nettles, saw palmetto, curcumin, and quercetin blend with antibiotic prulifloxacin | Serenoa repens associated with Urtica dioica and curcumin and quercitin extracts are able to improve the efficacy of prulifloxacin in bacterial prostatitis patients (R) | 14 days | Nearly 90% of patients who took prulifloxacin with natural treatments had reduced symptoms; after 6 months, all patients in this group had no recurrence of the disease | The association of S. repens, U. dioica, quercitin and curcumin extracts is able to improve the clinical efficacy of prulifloxacin in patients affected by CBP |
Closing thoughts
Lab testing is the first step if you suspect you have an issue with your prostate, or if you’re interested in taking a proactive role in keeping it healthy.
If you’re 40 or younger and have low PSA, it’s likely your prostate issue is fungal.
If PSA is elevated, more traditional paths are worth looking into, possibly even antibiotics, especially when they are paired with the nutrients listed above. But don’t rely on a pill of any kind. The goal is to change lifestyle factors that are contributing to a low grade infection. On this path, understanding blood type is important as it may determine the amount of animal protein you can handle.
Per the Washington University study, take a look at the acidity of your urine. If it’s highly acidic, you may have the perfect recipe for E. Coli colonization. Transitioning to a vegetarian diet could be what your body needs to alkalize your urinary tract which will have the effect of making it harder for pathogenic bacteria to thrive. You may also want to consider potassium citrate to accelerate this goal, especially if you find yourself taking biofilm disrupting supplements, such as NAC, that are highly acidic.
But don’t stop with antioxidants. Assuming you find high-quality strains that work for you, using probiotics will help to crowd out the bad guys. Strains I would look at: B. Longum, L. Plantarum, soil-based probiotics such as Prescript Assist, and even non-pathogenic yeast strains like S. Boulardii.
Last, gut health must be a focus for all men, especially in these circumstances. Embarking on a protocol to heal the gut could be just what the doctor ordered to shut down issues with leaky gut and the autoimmunity that goes with it.


i am at the end of in trying everything
surely there is a cure or relief for this horrible problem
tom
dublin
Superb analysis. Investigate the endocannabinoid palmitoylethanolamide (PEA) which covers many of the same bases discussed here and perhaps at a higher level of potency. Honokiol and luteolin may provide additional productive leads. Caveat: anecdotally, honokiol, which, among other things, is showing significant promise in some cancers, may have serious adverse effects in those with Gilbert’s Syndrome.
You know 98 % of men don’t have a clue on how complex & complicated the prostate is ? ? ? And either do doctors & even uroligist ? And i know having just been to one ? We put people on the moon ( i think ? ) and we have all this technology ( BUT WE STILL DON’T KNOW ABOUT THE PROSTATE ? ) Is it just job security for medical industry, i mean just the psa test is a cash cow ! Well john any wisdom you have is greatly appreciated !!!!!! Thanks. Dam prostate is one complexed organ. Like i said why should they fix it its one hell of a cash cow ! ! ! And when your desperate your desperate.
Excellent article – really valuable research and common sense. I am not sure what helped me in my 1st prostatitis but tried intra-prostatic injections of antibiotics in Rome, multiple oral and one I.v. antibiotic, autovaccines, bacteriophages, 25g of vitamin C i.v. for a month, my symptoms were diminishing after each of the above treatments, but eventually physical therapy cured me. The PT approach was recommended by a Swiss clinic as I am in Europe, pelvic floor relaxation and painful internal and external trigger-point release. Basically my remaining symptoms (annoying but still present) disappeared after 10 sessions, 1 hour each. I had a major improvement right after the 1st session, especially related to the frequency.
The study publish in the Central European Journal of Urology that you pointed out is interesting indeed but sadly they do not even mention the dosage of Fluconazole that was administered in their study, same applies to potassium citrate that was added to the anti-fungal protocol. In other studies I read that the daily dosage was usually 400mg for Fluconazole. Anti fungal diet is also critical. While doing all my ABX and other treatments I remained on gluten-free, diary-free diet and avoided carbohydrates, and of course sugar. Green tea and some herbs may also help. Physio Therapy is something I did not even consider during my long-term (2 years) prostatits… and I was wrong. One more note to you guys – do not trust a single lab , go to 2 -3 labs, find a university lab, and give all the samples to be tested, not just urine (semen cultivation and pcr dna are critical), including anaerobes. To recognize which lab is genuine, when they do anaerobic cultivation – you have to deliver a sample in a siringe , with no oxigen – i.e. semen. So you use a sterile container from a pharmacy, after washing penis and urinating – you have to ejaculate to the container and use 2ml syringe to take the semen, block syringe with a standard, unopened needle, and deliver to the lab within 30 minutes. At least that is the instruction I was given from the university lab. Cultivation lasted for 20 days, and results were provided with ABX sensitivity report. Clindamycin was ordered for my anaerobe. All other tests I’ve done were negative for anaerobes in 3 other commercial labs.. and they cultivated for 5 days. If you do not have a way to do that king of testing, trying clindamycin 300mg, every 8 hours may be beneficial if you tried standard antibiotics (cipro, levo, doxy, azithromycin), take probiotics 2h after antibiotics, ideally strong ones like VSL#3, and sacharomyces boulardi as well. Fluconazole can also be taken to prevent fungal overgrowth and – keep anti-fungal diet. Sorry for an unstructured comment but it’s hard to edit it here.
I was wondering if this therapy could help me too , what were your symptoms of prostatits ?? since my only symptom is frequent urination that is driving me crazy especially during the night , i wonder if this treatment could halep me out . Let me know please what were your symptoms so i know if its worth a try of this therapy Thanks Alberto
As I wrote, you should do the Lab tests – and not just urine in the first place (semen + urine cultivation for aerobic and anaerobic bacteria, semen PCR DNA – urogenital panel for all pathogens — to do all tests, you might have to split it into 2 visits unless you produce a lot of semen). If you rule out infections, you can go to a physio specializing in pelvic floor. If you are 45+ doing hormonal blood tests is also recommended to see if your hormones are OK. Urologist with TRUS trans rectal usg is always a good idea if you have never done it. Physio is the last stop at least it was for me – and I am glad I went there with all clean lab results. Symptoms that remained before physio were: frequent urination, and sometimes burning in the rectum). Physio was extremely painful.. internal and external. Give it a try, there is no harm getting assessed by a specialist. If you won’t see improvement after 3 sessions, simply stop going.
why physio was painful ??? i d like to know what are they doing ??and where did u go???
I had unprotected sex hundred days ago The doctor put me on three different antibiotics
And prostate pq
He took my urine and blood test negative I have burning and stinging at the tip of my penis and when I pee it dribbles I’m 60 years old
And I have no desire to have sex
I was diagnosed with prostitis and urethritis it is not going away
Hundred days doctor still has me on antibiotics any suggestions
Any drug for acute Prostatitis caused by bacteria? Currently using augumentin and doxycycline and vitamin c with zinc but not that effective
Prostatitis, what is it? We really don’t know. Was diagnosed of acute Prostatitis. I was put on augumentin and doxycycline. I used this prescription for approximately 6 weeks without stop. But when I stopped for 5 days the symptoms came back even worse. Am confused and scared as I just got married and wondering how this will affect having a child. Just got back on my medication and feel a little better. Don’t want to go to the urologist again as he will subject me to a whole lots of test again cos he warned me not to stop my medication. Who has an idea for acute Prostatitis caused by bacteria? What antibiotics or drug will rid the painful and depressing life. I will appreciate comments please. Am 35 years newly married and this illness seems to be getting the better part of me. I just want it gone already
prostatitis…. I took so many antibiotics and prostate kept getting worse, peeing 80 times a day 1/2 ounce at a time. They wanted to remove prostate. Idiots. Found out it was fungal infection not bacterial caused by antibiotics. Went to doctor in manila and he milked the prostate every day for ten days. The first 6 days I was screaming it hurt so bad. It only lasted 5 minutes per session.and on tenth day back to normal. He had. milked out the infection. I get a flair up usually once a year and have girl friend massage and it goes away. And to think doctors wanted to remove my prostrate and ruin my life. Dumbbells
One strain that doctors don’t test for is bacterial vaginosis! Guess what…they have to dip your urine in the female test kit!! And the stupid two day culture lab never shows anything!!! You have to demand a doctor to culture your urine for 5 days!!! Then you will find the bacteria!! Trust me when I say this….go find a doctor that will do this for you…and im speaking to everyone….then after do antifungal treatments…..also Cipro and levaquin and bactrim do not treat bacterial vaginosis and strep Veridian strains…only “clyndamacin” treats BV! And Veridian with doxycycline… Which nobody gets prescribed in prostate protocols…and another strain that gets in the prostate is negative staph coculyse if I’m spelling that wrong I apologize….I speak from experience…at this point I’m probably dealing with fungal issue with prostate…but penatration of fungal prescription have poor penatration into prostate…good luck everyone… hopefully I helped one person here and passed the karma….also NCIS has the real studies…but in doctor language…but read it anyways…
The # 1 and oft times only cause of inflammation in the human body is ………INFECTION !
Just because we can’t specifically identify the culprit doesn’t mean squat ! Read the story behind H.pylori and you’ll see that right out in the open is often a good place to hide The single largest cause of all prostate infection and inflammation is good old Chlamydia ! It does not culture well and is so quickly adaptable that many times it won’t culture at all. It took 21 years before my Chlamydia was identified.I have been in constant back and leg pain since
1974 with tons of nausea , burning , frequency and fatigue just for good measure ! The prostate along with the thyroid are the two most misdiagnosed and glaring mistakes made by
American Medicine ! With those two they miss their motto of ” Do no harm ! “
After reading your article i am more confused than ever. What is a the real cure or how can i stop the flares? I am in terrible burning stinging sensation in the urethra perianal area when urinating and and ejaculating also it feels like I have a gulf ball stuck in there. I am 31 do not drink do not smoke do not eat red meat. My urine test cameback negative my sti negative 3 urines and all negative normal ct scan. The stinging sensation is driving me crazy and preventing me from having sex with my wife.
Get a Semen Culture Done
Like John has already suggested get your PSA level tested. If PSA are low then it could be fungal infection. If PSA is high then its likely bacterial infection.
You can get a stool test done as well for fungal infections.
For fungal infection you need to go on Candida complex diet for atleast a couple of months and also need to take anti fungal medications. Flucunazole etc. You can also try some natural anti fungal treatment like Oregano oil and Caprylic Acid etc.
In either case, I recommend you start taking Quercetin. There is a supplement called ProstaQ which is really good and contains Quercetin and other useful ingredient. Give it a go it should at least reduce your symptoms.
Hi,
My father is suffering from severe burning sensation while passing the urine since 10 years. he undergone 3 operations since last 5 years. Frist laser operation to remove the extra growth , 2nd for the cyst and not sure about 3rd one. Now since 5 days urine is blocked. Test is done to see if the bladder is storing the water by injecting the water from outside using the tube. pressure is applied by patient and the flow rate. Bladder is normal , pressure is normal, flow rate is nil. Cystoscope is done today. don’t know the result yet. He is diabetic since 20 years, BP and cholesterol. Before to this he was having infections and taking antibiotics to relieve the pain. This time the urinary track is completely blocked. Just before to this he had sever gastic problems. He was taking antacids. Consume non veg once in a month. Veg food is India spices. Gastric problem is there since child wood.
Please guide me what are test to be made to find the bacterial infections. what supplements should be taking if there is a gut infections if its causing the inflammation.
I have written in layman language.. appreciate your help here