Smith-Lemli-Opitz Syndrome and Cholesterol: What You Need to Know
In this series of articles on cholesterol, I’ve already looked at whether cholesterol can be too low (spoiler alert! It can!). In this article, I look at one key cause of low cholesterol, Smith-Lemli-Opitz syndrome (“SLOS”).
Primary hypocholesterolemia and SLOS
Primary hypocholesterolemia occurs when there’s a genetic mutation in the pathway of cholesterol absorption, biosynthesis or metabolism. Some of the most common causes are:
- Abetalipoproteinemia
- Hypobetalipoproteinemia
- Tangier disease
- Chylomicron retention disease
- Inherited disorders of cholesterol biosynthesis.
Included in this last one is an autosomal recessive condition called Smith-Lemli-Opitz syndrome (SLOS).
What is Smith-Lemli-Opitz syndrome (SLOS)?
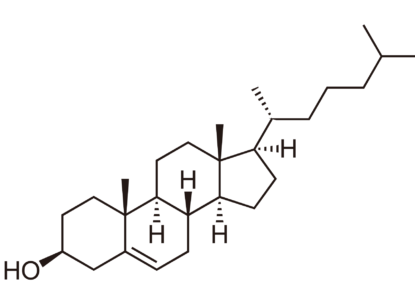
People with SLOS carry a mutation in the DHCR7 gene that encodes the enzyme 7-dehydrocholesterol reductase. The severity of symptoms of SLOS depend on the exact nature of the genetic mutation in DHCR7.
Current classifications for SLOS are mild, classical, or severe SLOS, based on cerebral, ocular, oral, and genital defects.
Some classic signs and symptoms of SLOS include:
- Small head size and narrow distance between temples
- A short, upturned nose
- Extra toes or fingers and/or fusion of toes and fingers
- Cleft palate
- Ambiguous genitalia
- Decreased frontal lobe size
- Congenital heart defects
- Kidney, pulmonary, liver, and eye abnormalities.
Because of significant overlaps in behaviors, some people with SLOS may initially be diagnosed with autism. An estimated half to three-quarters of people with SLOS also meet criteria for an autism diagnosis. Behaviors may include hypersensitivity to auditory and visual stimuli, self-injury, sleep disturbances, aggressive behavior, hyperactivity, hand-flicking, and stretching of the upper body.
In infants, SLOS may show up initially as a problem feeding or feeding intolerance. This may be due to physical malformations affecting the ability to suck and swallow. Infants with SLOS may also have higher than normal caloric demands due to a faster metabolic rate. Ear infections, pneumonia, and other recurrent infections are also associated with SLOS.
What causes SLOS?
SLOS is an autosomal recessive disorder, with more than 130 different types of mutations identified as causative. Most of these (around 87.6%) are single nucleotide polymorphisms or missense mutations.2 The result is a reduction in enzyme function but not a complete lack of or inhibiting of the enzyme. Less common are null mutations where the enzyme is completely lacking or completely dysfunctional.
As you might expect, the less impactful mutations are more common, given that more serious inhibition of the enzyme has more severe and potentially fatal results.
The most frequently reported mutation in DHCR7 is a switch from G to C in IVS8 (R). This mutation is a nonsense mutation where 134 nucleotides are inserted into the transcript of the gene. Those carrying two copies are severely affected, hence why they would be most likely to come to medical and scientific attention.
Who is at risk for SLOS?
So, who is most likely to carry the mutation just mentioned? Well, it seems the G to C switch was first reported in the British Isles and that around 1.09% of Caucasians of European heritage carry at least one copy of the allele.
Other mutations are less common and include a switch from C to T at 278. The effects of this are less severe in most cases. This 278C>T mutation is most common in people of Italian, Cuban, and Mediterranean descent.
Another nonsense mutation (452C>A) is the third most common affecting DHCR7. This mutation results in no DHCR7 enzyme being synthesized. This is most common in Northern Europe.
What can you do if you have a faulty DHCR7 gene?
A mutation in DHCR7 can affect your ability to synthesize cholesterol. If your diet lacks cholesterol, this might spell trouble. And, if you have trouble digesting and absorbing cholesterol, you may need a higher dietary intake to maintain a good pool for ongoing use.
Fortunately, most human bodies are pretty efficient when it comes to cholesterol absorption, with effective uptake in the gut and handy mechanisms for reabsorption of cholesterol. However, just because you consume cholesterol doesn’t mean it significantly affects the level of cholesterol in your blood. Your genetics and other dietary and lifestyle factors influence blood cholesterol far more than dietary cholesterol intake.
In fact, even though a high cholesterol intake (through diet and supplements) is part of treatment for SLOS, this isn’t always all that effective. Doses for treatment typically begin at 40-50 mg per kg of body weight per day. So, unless you prioritize foods with a very high cholesterol content, you will likely require a supplement providing purified food grade cholesterol.
Supplementing with cholesterol does not fully resolve the problem, though. For one thing, dietary cholesterol does not cross the blood-brain barrier, so it cannot support the requirement for cholesterol in brain tissue. Additionally, SLOS leads to an accumulation of the precursor to cholesterol, 7DHC, which can have toxic effects.
7DHC and lipid peroxidation
7DHC is incredibly reactive, making it extremely prone to lipid peroxidation. This increases systemic oxidative stress, destroying cell membranes and organelles. Unsurprisingly, then, antioxidants are often part of the treatment regimen for SLOS. Vitamin E appears to be particularly effective in helping to combat lipid peroxidation affecting 7DHC. 3
Oxidation isn’t the only issue with 7DHC, though. This intermediary metabolite is also known to impair intracellular cholesterol transport and to increase the degradation of 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) reductase, the enzyme involved in the rate-limiting step of cholesterol synthesis.
7DHC and simvastatin for cholesterol… deficiency?
Now, this is where things get a tad confusing. One proposed treatment for SLOS is the use of HMG-CoA reductase inhibitors. While this may seem nonsensical at first, given that the body needs this enzyme in early stages of cholesterol synthesis, it makes sense when we realize that HMG-CoA reductase is also the enzyme involved in the production of 7DHC. So, by inhibiting the activity of this enzyme, we can reduce the amount of 7DHC being produced, while simultaneously supplementing with readymade cholesterol.
As such, simvastatin use has been associated with decreases in 7DHC levels. Interestingly, simvastatin is also associated with increases in cholesterol. This, likely because the drug increases the expression of DHCR7. Yep, the drug that is prescribed to reduce cholesterol actually, well, supports cholesterol production. Hm.
Of course, simvastatin can only have this effect if a person has a functional copy of the DHCR7 gene. Otherwise, there’s no meaningful effect on cholesterol of increasing the gene’s expression. The use of simvastatin may, however, have toxic effects in people with no DHCR7 activity, illustrating just why it’s important to know your genotype before taking certain drugs.
Are you lost yet? Stick with me. Here’s a very basic diagram of where all the things I’ve just mentioned fit into cholesterol metabolism.
Enzyme à Metabolite à Gene/Enzyme à Cholesterol
HMG-CoA 7DHC DHCR7
[Inhibited by [Increased by
Simvastatin] Simvastatin]
Cholesterol metabolism is clearly far more complex than this diagram would suggest, but it should give you an idea of how one drug could have seemingly opposing effects. This explanation also helps provide a foundation for another piece of the puzzle: cholesterol hyper-absorbers and hyper-responders.
The takeaway
If you’re diagnosed with SLOS, your ability to synthesize cholesterol is, to some degree, compromised. This can affect the health of your cells and tissues and your ability to synthesize vitamin D, bile acids, and hormones. You may be able to avoid dangerously low cholesterol levels by eating a diet high in cholesterol, or you may need to take a pure food grade cholesterol supplement. In some cases, your doctor may prescribe simvastatin or other medications to help reduce the adverse effects of toxic metabolite 7DHC.