5 Key Causes of Low Cholesterol, and Why it Matters
Genes Mentioned
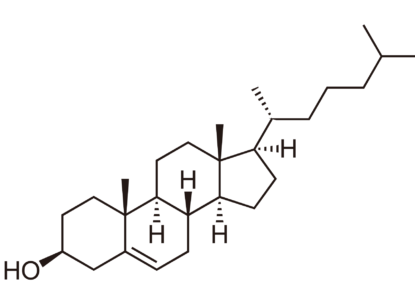
Cholesterol is an essential component of cell membranes and a precursor to steroid hormones, vitamin D, and bile acids. Thankfully, the body makes 80% of its cholesterol “in-house,” which means the vast majority of us make enough cholesterol to meet daily needs and keep our cells and tissues happy.
For some, though, cholesterol deficiency is a real concern.
Below are 5 key causes of low cholesterol, and why it matters.
What causes low cholesterol?
Doctors classify low cholesterol as primary or secondary hypocholesterolemia. Primary hypocholesterolemia occurs when there’s a genetic mutation in the pathway of cholesterol affecting:
- Cholesterol absorption
- Cholesterol biosynthesis
- Cholesterol metabolism.
Some of the most common causes are thought to be abetalipoproteinemia, hypobetalipoproteinemia, Tangier disease, chylomicron retention disease and inherited disorders of cholesterol biosynthesis, such as an autosomal recessive condition called Smith-Lemli-Opitz syndrome (SLOS), which I look at in more detail here.
Secondary hypocholesterolemia can occur due to: 1
- Anemia
- Hyperthyroidism
- Malignancy
- Liver disease
- Malabsorption
- Malnutrition
- Infection
- Chronic inflammation
- Critical illness
- Serious stress
- The use of some drugs (hello, statins!).
So, what are the 5 most common causes of high cholesterol? Chances are they’re:
- Genetic polymorphisms and conditions such as SLOS
- Statins!
- A zero-cholesterol diet (i.e. veganism)
- Acute illness
- Older age.
Let’s briefly look at each of these and offer a few quick solutions.
1. Genetic polymorphisms and SLOS
A whole host of genes are involved in cholesterol synthesis, absorption, and metabolism. These include LDLR, PCSK9, and APOB, which affect cholesterol clearance. Mutations in these genes almost always results in high cholesterol levels, but in a few cases, mutations may result in a total deficiency of PCSK9 and LDL-C levels in the range of 15 mg/dl without any reported adverse effects. 2
More commonly, mutations in the DHCR7 gene cause very low cholesterol and can lead to Smith-Lemli-Opitz syndrome (SLOS). The DHCR7s gene is essential for proper cholesterol synthesis, and if someone has a mutation in this gene, they may have serious abnormalities at birth and ongoing challenges. In some pregnancies, a mutation in DHCR7 can lead to spontaneous abortion.
Even if your genetic tests show a mutation affecting DHCR7, you may only have mild reductions in cholesterol synthesis. It all depends on the type of mutation. In these cases, a diet including cholesterol-rich foods can help, or you may be advised to take a cholesterol supplement.
2. Statins
The whole point of statins is to reduce cholesterol, but there’s real concern that statins are prescribed willy-nilly, especially for older folks. And, given that older age is one of the potential causes underlying low cholesterol, it’s always smart to get your lipids checked regularly and not just accept your doc’s outdated one-size-fits-all ideas about statins.
3. A zero-cholesterol diet
Dietary cholesterol comes exclusively from animal-derived foods, so if you don’t eat much or any dairy, eggs, meat, or fish, chances are you have a low or zero intake of cholesterol. Unlike, say, vitamin C, however, the human body is, under normal circumstances, capable of producing all the cholesterol it needs. This means that cholesterol is not classed as an essential nutrient, for most people.
That said, if your ability to create your own cholesterol is compromised in some way, such as having SLOS, and your diet lacks cholesterol, then you might be in trouble. And, if you have trouble digesting and absorbing cholesterol, you may need a higher dietary intake to maintain a good pool for ongoing use.
Anecdotally, some folks who eat a very low or zero cholesterol diet experience more pronounced periods of depression, anxiety, and general low mood than they did when eating foods containing cholesterol. (More on this below!)
4. Acute illness
Severe infection and acute illnesses have been linked to temporary reductions in cholesterol. Seemingly, even minor illnesses also nudge cholesterol down a little, by about 5 mg/dL. This was first documented in people with tuberculosis, where the lowest levels of cholesterol were associated with a higher risk of death from the infection.4
Accordingly, doctors are now looking into whether it’s a good idea to try to increase cholesterol levels in people with sepsis. Once again, given the increased vulnerability to infection in older age and possible reductions in cholesterol absorption and synthesis, older adults would be smart to pay attention to their lipid levels.
5. Older age
Finally, as mentioned a few times already, getting older can be an underlying factor in low cholesterol levels. As with many aspects of health, older age can affect the body’s ability to synthesize certain substances, and cholesterol is no exception.
Research shows a reduction of cholesterol synthesis with aging but, importantly, this is associated with increased circulating cholesterol levels, not decreased levels. 5 Why? Possibly because other mechanisms also go awry with age. In older adults who already have a propensity for low cholesterol, though, decreased synthesis could cause problems related to cholesterol levels being too low. Speaking of which….
When is cholesterol too low?
There’s no consensus on how low is too low for cholesterol. The Mayo Clinic suggest that LDL cholesterol is very low if less than 40 mg per deciliter of blood. Even then, there are no confirmed risks to very low cholesterol. And, any risks would also have to account for other factors, such as lipid peroxidation, antioxidant status, and other blood lipid levels.
Most doctors still consider a level of 70 mg/dL as the target to help their patients reach by using statins and other medications. Even at this LDL-C level, though, there’s still an increased risk of cardiovascular events. So, as with so many things, how low is ‘too low’ depends on the individual.
Symptoms of very low cholesterol
We need cholesterol for healthy cell membranes, bile acid production, and the production of vitamin D and hormones. Too little cholesterol in early development can cause genital malformations and reproductive abnormalities. Low levels of cholesterol in later life can also affect steroid sex hormone production and reproductive health in puberty and beyond.
In extreme cases (such as SLOS), abnormally low levels of cholesterol production can cause fatal malformations in fetal development and early infancy. 1 In children who survive, cognitive and behavioral disabilities are common, with varying degrees of severity.
Low cholesterol has also been linked to an increased risk of preterm birth.6 However, cholesterol levels tend to increase in pregnancy as does Apolipoprotein B, likely because cholesterol is an important component in steroid sex hormones.78 Cholesterol can cross from maternal to fetal circulation; we know this because cholesterol has been found in fetuses severely affected by SLOS, to the extent that the fetus was unable to produce any cholesterol.
Some research suggests, however, that even when cholesterol levels are extremely low, the body still manages to maintain steroid hormone and bile acid production, and the cholesterol blood-brain barrier protects cells in the central nervous system.9
What about if your cholesterol is just a little bit lower than normal?
The jury’s still out on what happens if you have cholesterol levels a bit lower than average but not extremely low.
Demographic research suggests that mortality is higher at the extreme ends of cholesterol status: too high or too low and you’re more likely to die sooner.10 However, it might well be that low cholesterol isn’t so much a cause of a decline in health and eventual death as an effect itself, i.e. whatever else is raising your risk of disease might also cause a drop in cholesterol.11 Or, it could simply be coincidence.
Interestingly, low levels of cholesterol have also been associated with hemorrhagic stroke, although further study is needed to fully understand this possible link. In one study, people with total cholesterol levels below 160 mg/dL who had an intracerebral hemorrhage (ICH) were 80% more likely to have more severe neurological deficits. What’s more, those with total cholesterol levels below 160 mg/dL who had a Body Mass Index below 22 were almost four times more likely to die within three months of the stroke.12 A more recent meta-analysis suggests that APOE4 and APOE2 also have a large role to play in determining the risk of ICH and outcomes.13
Low cholesterol, depression, and anxiety
There’s very little research to link low dietary cholesterol to changes in mental health. There’s no clear evidence suggesting that reducing your total cholesterol will make you depressed and anxious.
What the evidence does suggest is a link (causative or not) between low serum cholesterol and the risk of depression and anxiety. Again, it’s worth stressing that low cholesterol could be a result of poor mental health or be linked in some other way. Inflammation has been linked to both depression and low cholesterol, for instance.
That said, researchers are hard at work investigating this potential link. In one study, researchers looked at the lipid levels of 121 healthy young adult women and found that a higher score on the Neuroticism, Extraversion, Openness-Personality Inventory (NEO-PI) depression subscale was associated with lower total cholesterol, triglycerides, and the ratio of total cholesterol to HDL cholesterol.14 Anxiety scores were also linked to lower total cholesterol, triglycerides, LDL-cholesterol, and the ratio of total cholesterol to HDL cholesterol.
The significance remained even when adjusting for age, BMI, physical activity, oral contraceptive use, and hostility. More than a third (39%) of the women with low total cholesterol concentrations (<160 mg/dL) had higher depression scores, versus 19% of those with moderate to high cholesterol levels, and 35% (vs. 21%) had higher anxiety scores.
In another study, researchers found that fasting serum cholesterol levels were low in people with mixed manic bipolar disorder, especially during manic episodes, compared to the general population.15 And, again, lower cholesterol levels were significantly associated with major depressive disorder (OR 4.229) and suicide attempt (OR 5.540) in another study.16
The takeaway
Scientists have paid so much attention to the perils of high cholesterol that there’s relatively scant research into the risks of low cholesterol. In general, though, the research so far suggests that low cholesterol intake poses relatively little risk for most people. That is, of course, unless they have a genetic anomaly such as SLOS. Similarly, low serum cholesterol levels have not been conclusively linked to any serious health issues.
Very low levels of cholesterol may, however, be associated with an increased risk of:
- Depression
- Anxiety
- Symptoms of autism spectrum disorder
- Hemorrhagic stroke and poorer outcome from stroke
- Preterm birth and low birth weight if your cholesterol is low while you’re pregnant.
Concerned about low cholesterol? Before you start searching for a supplement, get your lipids checked by a reputable lab. Then you can compare them to the recommended cholesterol levels from Mayo Clinic.
You might also want to scrutinize your genome for variants in DHCR7, APOB, LDLR, PCSK9 and other genes involved in cholesterol metabolism. And, finally, check out my article on cholesterol-rich foods and learn more about the genetics and impact of SLOS here.